SCIENTIFIC INVESTIGATIONS
Anne G. Griffiths, MD1; Pallavi P. Patwari, MD2; Darius A. Loghmanee, MD3,4; Matthew J. Balog, RSPGT3; Irina Trosman, MD3,4; Stephen H. Sheldon, DO3,4
¹Children’s Respiratory and Critical Care Specialists, Minneapolis, MN; 2University of Illinois Hospital and Health Sciences System, University of Illinois College of Medicine, Chicago, IL; 3Ann and Robert H. Lurie Children’s Hospital of Chicago, Chicago, IL; 4Northwestern University, Feinberg School of Medicine, Evanston, IL
Study Objectives: Polysomnography is the gold standard for diagnosis and characterization of severity of sleep-disordered breathing. Accuracy and reliability of the technology used are critical to the integrity of the study’s interpretation. Strict criteria for obstructive sleep apnea in children are lacking and diagnosis often requires consideration of frequency of respiratory events in addition to other measures. Current American Academy of Sleep Medicine recommendations for pediatric patients includes use of respiratory inductance plethysmography (RIP) belts, whereas polyvinylidene fluoride (PVDF) belts are currently only acceptable for use in adults. We hypothesized that PVDF belts would be equally effective as RIP belts for detection of respiratory effort and events in children.
Methods: Children ages 2–17 y were recruited from a large pediatric tertiary referral center after obtaining consent for participation. Fifty subjects were recruited (average age, 7.8 y). Clinically relevant limits of agreement were predetermined to be a difference in total count of obstructive or central apneas or hypopneas of ± 5 events.
Results: Scoring of respiratory events was not significantly different by belt type based on Bland-Altman plots of total apnea-hypopnea index and obstructive apneas. Obstructive hypopneas scoring ranged beyond our clinical limit of agreement. Findings in obese subjects were consistent with the larger sample with the exception of an increase in outliers. Artifact amount was comparable (RIP 10.9% ± 22.5% and PVDF 10.5% ± 19.5%).
Conclusions: Based on these findings, PVDF belts appear to be as effective as RIP belts in detection of respiratory effort and events in children.
Commentary: A commentary on this article appears in this issue on page 159.
Keywords: obstructive sleep apnea, pediatrics, polysomnogram, respiratory monitoring, sleep-disordered breathing
Citation: Griffiths AG, Patwari PP, Loghmanee DA, Balog MJ, Trosman I, Sheldon SH. Validation of polyvinylidene fluoride impedance sensor for respiratory event classification during polysomnography in children. J Clin Sleep Med. 2017;13(2):259–265.
INTRODUCTION
Polysomnography is the gold standard for diagnosis of sleep- disordered breathing (SDB) and characterizing disease severity. In addition to careful history and physical examination, man- agement of SDB often hinges on the interpretation of multiple measured respiratory parameters used during a polysomnogram (PSG). The accuracy and reliability of the technology used dur- ing a PSG are critical to the integrity of the study’s interpretation.
Based on the update of American Academy of Sleep Medi- cine (AASM) Scoring Manual,1 in children, identification of respiratory events such as apnea and/or hypopnea requires oro- nasal thermal airflow sensor, nasal pressure transducer, respi- ratory inductance plethysmography (RIP), and carbon dioxide partial pressure (pCO2 ) monitoring. For evaluation of respiratory effort, esophageal manometry or dual thoracoabdominal RIP belts are recommended for use in children. Further, polyvi- nylidene fluoride dual thoracoabdominal belts (PVDFb) are also recommended sensors in detection of respiratory effort in adults, largely based on the work by Koo and colleagues demonstrating comparable detection of respiratory events of apnea and hypop- nea with polyvinylidene fluoride (PVDF) versus RIP monitor- ing.2 RIP technology has become the mainstay of respiratory event detection with widespread usage in polysomnography because of its noninvasive approach and accessibility in con- trast to the decreased practicality and invasiveness of esopha- geal manometry. PVDF technology is already an incorporated technology in oronasal thermal airflow sensors recommended for use in both children and adults.3 However, based on a lack of evidence for its use in pediatric polysomnography, PVDFb are not currently recommended for respiratory effort monitor- ing and event detection in children. PVDFb detect changes in impedance and are less position dependent compared to RIP belts (RIPb). RIPb require proper orientation to detect changes in cross-sectional areas during breathing to obtain accurate and interpretable information. RIPb require correct orientation, and their adjustment may interrupt the sleep of young patients and lead to interference in their natural sleep cycles and suboptimal study results. As PVDFb detect changes in electrical resistance without the polarity seen in RIPb positioning, PVDF may be a particularly attractive new technology for respiratory event sensors to be used in pediatric polysomnography.
We hypothesize that compared to RIPb, detection of respi- ratory events with PVDFb will allow for improved pediatric polysomnography interpretation, through decrease in artifact and increase in respiratory event recognition.
RESULTS
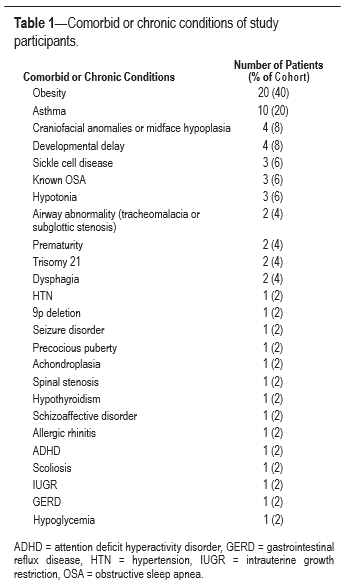
Subjects included 18 girls and 32 boys, ages 2.5 through 17.7 y (mean age 7.8). No subjects were excluded from participation based on the presence of chronic conditions. Eight subjects had a history of previous adenoidectomy and/or tonsillectomy. Of
our cohort, more than half of the subjects presented with un- derlying chronic or comorbid conditions, and many children had more than one chronic disease or congenital abnormal- ity (Table 1). The most frequent comorbid conditions included obesity (40%, n = 20), asthma (20%, n = 10), developmental delay (8%, n = 4), and craniofacial anomalies (8%, n = 4).
Interscorer reliability was high based on calculated percent concordance (approximately 98%) for the randomly selected eight studies scored by both sleep medicine physicians’ review.
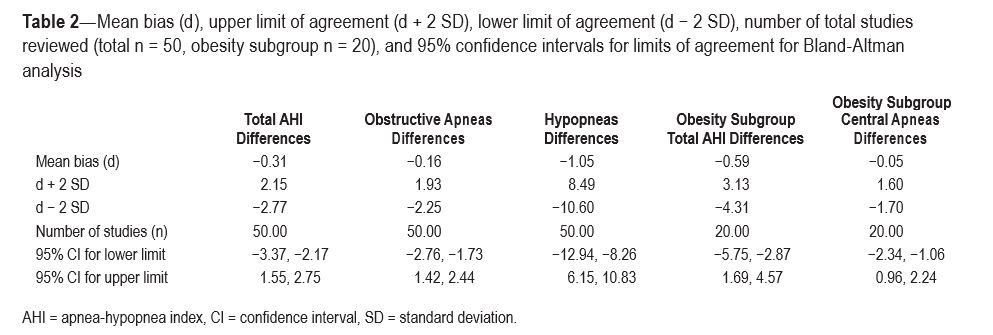
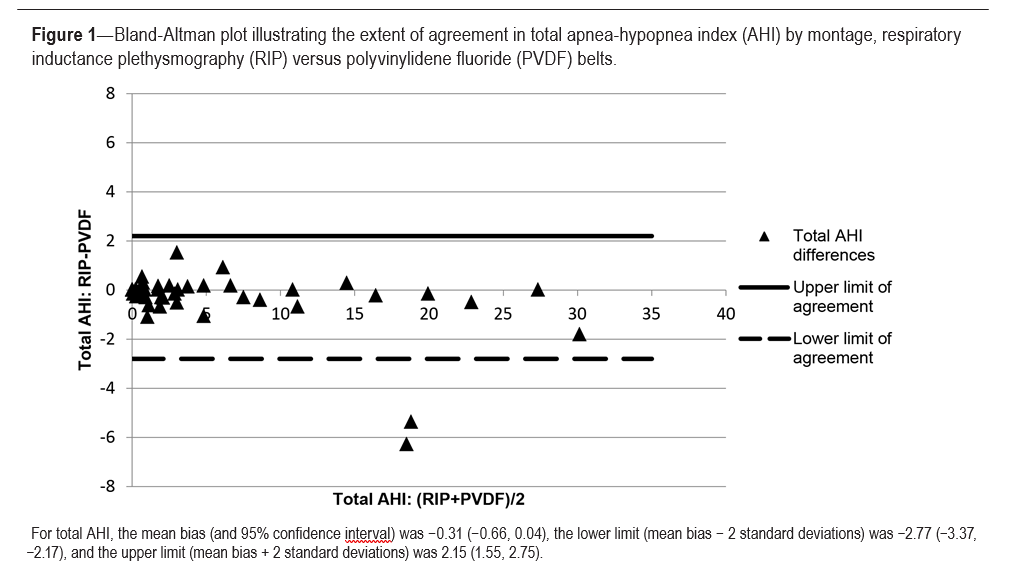
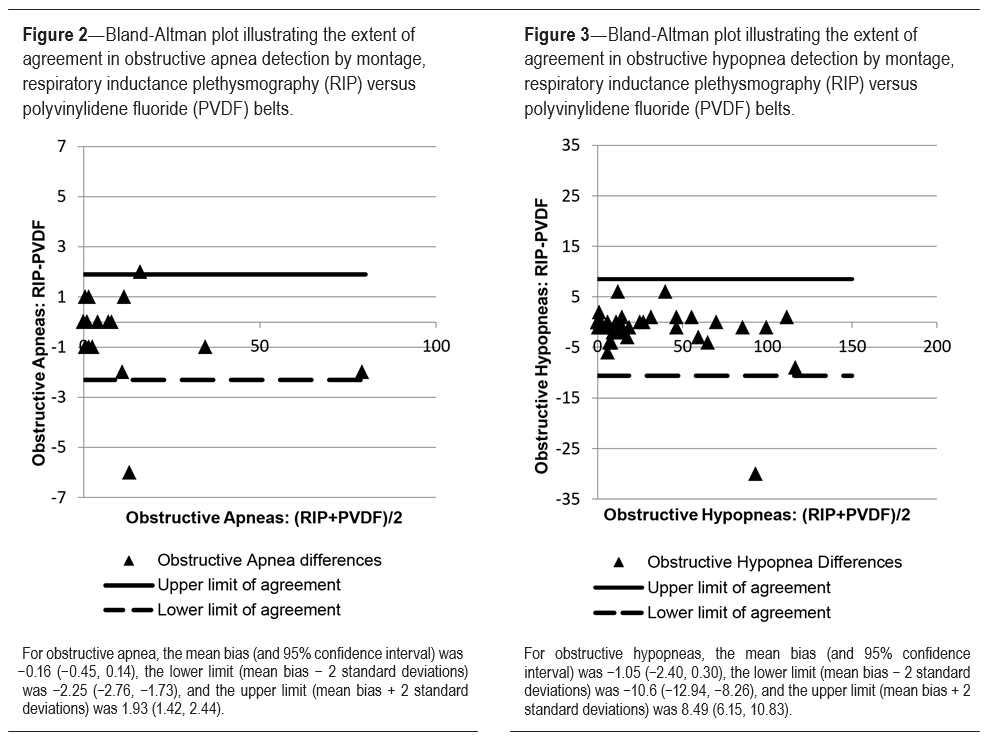
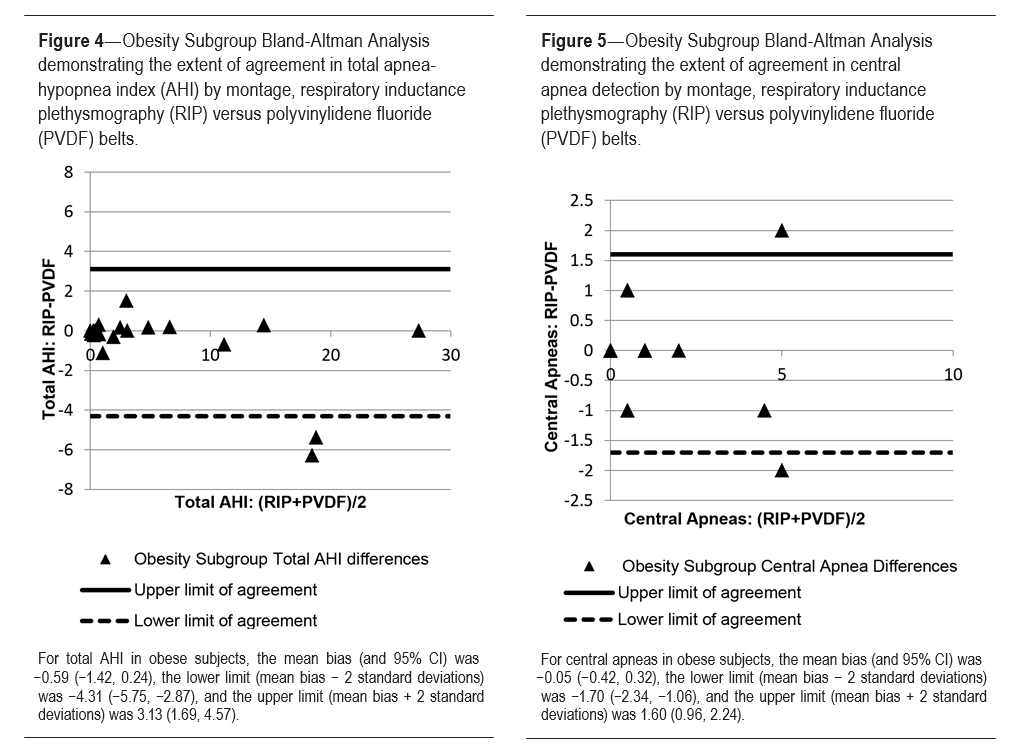
Bland-Altman plots were constructed and limits of agree- ment based on 2 SD of the mean difference were added to the plots for total AHI, obstructive apneas, and obstructive hypop- neas. No central hypopneas were scored. Subgroup analysis of total AHI and central apneas was performed for obese sub- jects. Mean bias (d), upper limit of agreement (mean bias +2 SD, lower limit of agreement (mean bias −2 SD), number of total subjects (n), and 95% confidence intervals for the limits of agreement of each Bland-Altman plot are listed in Table 2.
When looking at all included subjects in our sample, more than 95% of the data were contained within the limits of agree- ment (or within 2 SD of the mean) with relatively equal scatter on either side of the mean bias indicating no systematic bias between methods. The agreement between the montages using RIPb and PVDFb (demonstrated in Figure 1) for AHI is strong, with data tightly scattering on either side of the mean bias and contained within the limit of agreement by 2 SD and clinical criteria (less than ± 5). Outliers in AHI account for less than 5% of the data overall.
Figure 2 reveals similar results of total AHI determination and demonstrates a strong degree of agreement in obstructive apnea scoring between the two belt types (RIPb and PVDFb) for all study subjects. Evaluating obstructive hypopneas alone, the data demonstrate increased scatter beyond our clinically determined limit of agreement of greater than ± 5 events but still suggests no systematic bias between methods (Figure 3).
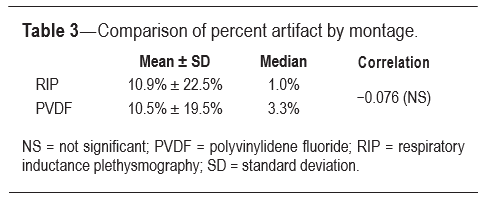
Subgroup analysis of total AHI in obese subjects did demon- strate a 95% confidence interval for the lower limit of agreement that crossed −5. In general the scatter is tightly surrounding the mean bias of −0.59 (± difference of 2 in AHI score) with the exception of the two outliers (accounting for 10% of the obese subgroup), which demonstrated an increase in AHI with PVDFb montage compared to with RIPb montage (Figure 4). Subgroup analysis of central apneas in the obese patients demonstrated outliers on either side of the limits of agreement by 2 SD criteria; however, they were not beyond our predetermined realm of clinically significant difference with scoring differences of ± 2 events. The scatter demonstrated in central apnea scoring in obesity does not favor one belt strongly over the other (Figure 5).The amount of recorded artifact was comparable between the PVDFb and RIPb montages, with artifact accounting for 10.9% of TST using RIPb (± 22.5% SD) and 10.5% of TST using PVDFb (± 19.5% SD), (Table 3).
DISCUSSION
This study directly compares respiratory effort sensing using RIP and PVDF technology in the pediatric population. Pedi- atric patients span a wide range of weights, heights, and other anthropometric parameters, requiring technology that can adapt for this. Infants in particular have small body surface area for proper belt placement. Bland-Altman analysis of belt performance in terms of re- spiratory effort overall demonstrated strong agreement without
BRIEF SUMMARY
Current Knowledge/Study Rationale: Current American Academy of Sleep Medicine recommendations include use of respiratory inductance plethysmography belts (RIPb) for detection of respiratory events in children and adults, whereas use of polyvinylidene fluoride belts (PVDFb) is only recommended for adults. With advances in quality of technology, we aimed to determine if PVDFb would be as effective as RIPb in the pediatric population.
Study Impact: Our study directly compares traditional RIPb technology and PVDFb technology for respiratory effort sensing in pediatric patients.
METHODS
This study was approved by the Institutional Review Board at Ann & Robert H. Lurie Children’s Hospital of Chicago. In- formed consent and assent (when appropriate) was obtained for all subjects. Fifty subjects ages 2 through 17 y who were scheduled for routine nocturnal polysomnogram4–7 were pro- spectively enrolled from September 2013 through February 2014, at the AASM-accredited Sleep Medicine Center at Ann & Robert H. Lurie Children’s Hospital, a tertiary referral cen- ter. Non–English-speaking patients or those with chronic dis- ease (such as recent major chest or abdominal surgery) that precluded safe participation were excluded.
In addition to routine monitors including conventional RIP belts (Protech, Murrysville Pennsylvania), PVDF belts (Dy- medix Diagnostics, Shoreview Minnesota) were placed on the chest and abdomen of the child per manufacturers’ guidelines. All PSGs were recorded and scored based on AASM criteria, using low-frequency filter (LFF)/high-frequency filter (HFF) settings of 0.3/35 Hz for all electroencephalography (EEG) and right and left electrooculography (EOG) leads, 0.3/70 Hz for the electrocardiography (ECG) leads, 10/100 Hz for electro- myography (EMG) at the chin, intercostal, right leg and left leg, and snore microphone, and 0.1/15 Hz for pressure trans- ducer air flow (PTAF), PVDF airflow nasal sensor, RIP belts, and PVDF belts. End-tidal pCO2 and oxyhemoglobin saturation (SpO2 ) were obtained via capnography and pulse oximetry.
After clinical interpretation of the PSG occurred, two copies of an unscored, deidentified study were created with coded file names. Each deidentified study included a single set of chest and abdomen belts (RIPb or PVDFb).
Cadwell’s Easy III acquisition software (version 3.14.2, Ken- newick Washington) was used with expanded (patients age 3 y or older) and regular (patients younger than 3 y) montages, which included bilateral EEG leads of Fp1, Fp2, Fpz, F3, F4, C3, C4, Cz, T3, T4, P3, P4, Pz, O1, O2, M1, M2 and Fpz, M1, T3, C3, Cz, C4, T4, M2, Pz, O2, respectively, EOG, EMG (submentalis, anterior tibialis), ECG with heart rate, continuous end tidal carbon dioxide monitoring with waveform, oxygen saturation with plethysmography waveform, PTAF channel facilitated by Salter Laboratories oral/nasal cannula (Lake Forest Illinois), and PVDF air flow sensor (Dymedix Diagnostics). Sleep stage was determined by a registered polysomnographic technologist for each 30-sec epoch.
Scoring of respiratory events was performed by two board- certified sleep medicine physicians (DAL, IT) who were blinded to belt type (RIP or PVDF). Each scorer reviewed 33 studies, 8 of which were randomly selected for duplicate scoring to determine interscorer reliability based on percent concordance. Each study was scored for respiratory events according to the AASM recommended Respiratory Rules for Children.7 The total number of respiratory events (central ap- nea, obstructive apnea, obstructive or central hypopnea), re- spective respiratory indices (central apnea index, obstructive apnea index, apnea-hypopnea index [AHI]), and diagnostic category (mild, moderate, or severe) were recorded. Prolonged expiratory apnea and post-sigh central apnea were excluded from analysis. Also, epochs with respiratory sensor artifact were counted and percentage of artifact based on total sleep time (TST) calculated. Epochs consisting of more than 50% artifact were counted as epochs of significant artifact that re- stricted interpretation for that time period.
In addition to respiratory measures, characteristics of the subjects were also entered into an Excel database and later ex- ported to Statistical Package for Social Sciences (SPSS) soft- ware for further statistical analysis. Statistics included Pearson correlation for artifact by montage. Preliminary Pearson corre- lation was performed to determine strong correlation between the two montages using RIPb and PVDFb; however, formal Bland-Altman plots were constructed to better characterize the agreement between montages utilizing RIPb and PVDFb, identifying trend lines for 2 standard deviations (SD) from the mean bias for each plot. Designated limits of agreement based on clinical relevance were identified by our sleep medi- cine physicians to be a difference in total count of obstructive apneas, obstructive hypopneas, and/or central apneas of ± 5 events. Subgroup analysis of belt agreement in obese subjects was also performed for total AHI and central apneas.
significant systematic bias. However, there was wider scatter of the data for the scoring of obstructive hypopneas overall in either direction (revealing no systematic bias), and weaker agreement was demonstrated as five comparisons crossed our clinical threshold of importance of ± 5 events. Hypopneas are often difficult events to score1 and belt type may not simplify that process for sleep medicine physicians The subgroup analysis of PSG scoring agreement in obese subjects was com-
parable to that seen in the larger sample, with the exception of wider limits of agreement by the 2 SD criteria and increase in outliers. Given the small sample size of the obesity subgroup, a larger sample in the future may help demonstrate whether or not systematic bias would be present in that population.
Parents of infants and developmentally delayed children often find polysomnographic testing to be distressing as their children may not sleep well, even with the least disruption pos- sible during testing. As volitional study participation and co- operation in pediatric polysomnographic testing is challenging, obtaining valid results with proper belt function is essential in avoiding repeated studies.
PVDF has been shown to demonstrate strong piezoelectric- ity to induce a dipole moment and can be manufactured into thin films. When the film is stretched, the molecular chains orient under tension. Unlike other piezoelectric sensors and strain gauges, PVDF compresses instead of expands (and expands instead of compresses when exposed to the same electrical field), making its stability a desirable feature.8 It should be noted that this is not the first application of PVDF technology in pediatric polysomnography. PVDF airflow sen- sors are a recommended modality for monitoring of airflow in both adult and pediatric patients according to the update of The AASM Manual for the Scoring of Sleep and Associ- ated Events.1 However, this application of PVDF technology in respiratory effort sensing belts was not recommended at the time of that publication.
Polysomnographic study of children poses some challenges that are distinct from those seen in adults. Classification of se- verity of SDB is more conservative in pediatric patients than in adults.7,9 Pediatric PSG scoring classifies greater severity of SDB based on frequency of events than scoring based on the adult recommendations for the same frequency of events. Un- like in adults, obstructive events are rare in children1 (high- lighting the importance of equipment accuracy for result validity and reproducibility).
CONCLUSIONS
Our study demonstrated that PVDFb appeared to be as effec- tive as the currently recommended RIPb in detection of respi- ratory effort and events in children. Further, the quantity of artifact was comparable between PVDFb and RIPb. Therefore, when used in conjunction with additional standard polysom- nographic monitoring equipment, PVDFb can be considered acceptable sensors for pediatric use
ABBREVIATIONS
AASM, American Academy of Sleep Medicine
ADHD, attention deficit hyperactivity disorder
ACKNOWLEDMENTS
The authors thank Dr. Mark Haupt and Dr. Denise Goodman for their contributions to this project.
Classification of disease severity should not be limited to AHI scoring, and treatment thresholds remain controver- sial.7,9–13 However, the recent American Academy of Pediatrics (AAP) Clinical Practice Guideline for pediatric obstructive sleep apnea diagnosis and management7 discusses considering pharmacotherapy in residual SDB that is designated as mild based on AHI cutoff. Our results emphasize the point that cau- tion should be used in interpreting PSG results in its contribu- tion to disease severity classification in clinical practice.
Contrary to our hypothesis that less artifact would be de- tected using PVDFb than with the use of RIPb, quantity of artifact was not statistically different. Although the amount of recorded artifact was comparable, it did not always occur in overlapping periods for PVDFb and RIPb, suggesting perhaps subtle differences in each belt’s susceptibility to artifact and signal disturbance.
Limitations to our study were identified. Many of our sub- jects had relatively mild SDB, which may have skewed our results due to fewer apnea or hypopnea events for analysis. Outliers existed between the two belt types. Nonetheless, they were not associated with poor technical quality or sig- naling uses. Additionally, our study was not designed to look at how often the registered polysomnographic technologist interrupted testing to reposition PVDF versus RIP belts. Our center does not use summation belt effort data as a surrogate for airflow, and thus belt summation data were not analyzed in this study. In the pediatric population it would be helpful to look at belt agreement in a larger sample of subjects with skeletal deformities because our study was limited in number of such individuals. Furthermore, overall this was a small co- hort comparing relatively new equipment and we are unable to comment on whether either belt type would more likely be- come damaged or unusable overtime. A difference in cost and durability may be present. Analysis of price differential and durability was beyond the scope of this project but may be an important consideration in employing various methodologies in the sleep laboratory.
AHI, apnea-hypopnea index
CI, confidence interval
ECG, electrocardiography
EEG, electroencephalography
EMG, electromyography
EOG, electrooculography
GERD, gastrointestinal reflux disease
HFF, high-frequency filter
HTN, hypertension
IUGR, intrauterine growth restriction
LFF, low-frequency filter
OSA, obstructive sleep apnea
pCO2, carbon dioxide partial pressure
PSG, polysomnogram
PTAF, pressure transducer air flow PVDF, polyvinylidene fluoride PVDFb, polyvinylidene fluoride belts
RIP, respiratory inductance plethysmography
RIPb, respiratory inductance plethysmography belts
SD, standard deviation
SDB, sleep-disordered breathing SpO2, oxyhemoglobin saturation TST, total sleep time
SUBMISSION & CORRESPONDENCE INFORMATION
Submitted for publication March, 2015
Submitted in final revised form August, 2016
Accepted for publication October, 2016
Address correspondence to: Pallavi P. Patwari, MD, Medical Director, Pediatric Sleep Medicine, Rush University Children’s Hospital, Chicago, IL 60612; Tel: (312) 942-6194; Fax: (312) 942-6145; Email: Pallavi_Patwari@rush.edu
DISCLOSURE STATEMENT
In-kind donation of PVDF belts for use in this study was provided by Dymedix Diagnostics Inc. Dr. Sheldon has functioned as pediatric consultant to Dymedix Diagnostics, Inc. All work was performed at Ann & Robert H. Lurie Children’s Hospital of Chicago. The other authors have indicated no financial conflicts of interest.
Figure 2 reveals similar results of total AHI determination and demonstrates a strong degree of agreement in obstructive apnea scoring between the two belt types (RIPb and PVDFb) for all study subjects. Evaluating obstructive hypopneas alone, the data demonstrate increased scatter beyond our clinically determined limit of agreement of greater than ± 5 events but still suggests no systematic bias between methods (Figure 3). Subgroup analysis of total AHI in obese subjects did demon- strate a 95% confidence interval for the lower limit of agreement that crossed −5. In general the scatter is tightly surrounding the mean bias of −0.59 (± difference of 2 in AHI score) with the exception of the two outliers (accounting for 10% of the obese subgroup), which demonstrated an increase in AHI with PVDFb montage compared to with RIPb montage (Figure 4). Subgroup analysis of central apneas in the obese patients demonstrated outliers on either side of the limits of agreement by 2 SD criteria; however, they were not beyond our predetermined realm of clinically significant difference with scoring differences of ± 2 events. The scatter demonstrated in central apnea scoring in obesity does not favor one belt strongly over the other (Figure 5). The amount of recorded artifact was comparable between the PVDFb and RIPb montages, with artifact accounting for 10.9% of TST using RIPb (± 22.5% SD) and 10.5% of TST using PVDFb (± 19.5% SD), (Table 3).
REFERENCES
1. Berry RB, Budhiraja R, Gottlieb DJ, et al. Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med. 2012;8(5):597– 619.
2. Koo BB, Drummond C, Surovec S, et al. Validation of a polyvinylidene fluoride impedance sensor for respiratory event classification during polysomnography. J Clin Sleep Med. 2011;7(5):479 – 485.
3. Berry RB, Koch GL, Trautz S, Wagner MH. Comparison of respiratory event detection by a polyvinylidene fluoride film airflow sensor and a pneumotachograph in sleep apnea patients. Chest. 2005;128(3):1331–1338.
4. Roland PS, Rosenfeld RM, Brooks LJ, Friedman NR, Jones J, Kim TW. Clinical practice guideline: polysomnography for sleep-disordered breathing prior to tonsillectomy in children. Otolaryngol Head Neck Surg. 2011;145(1Suppl):S1–S15.
5. Aurora RN, Zak RS, Karippot A, et al. Practice parameters for the respiratory indications for polysomnography in children. Sleep. 2011;34(3):379 –388.
6. Aurora RN, Lamm CI, Zak RS, et al. Practice parameters for the non- respiratory indications for polysomnography and multiple sleep latency testing for children. Sleep. 2012;35(11):1467–1473.
7. Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2012;130(3):e714–e755.
8. Kawai H. The piezoelectricity of poly (vinylidene fluoride). Jpn J Appl Physics. 1969;8:975.
9. Iber C, Ancoli-Israel S, Chesson A, Quan SF. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007:48– 49.
10. Marcus CL, Omlin KJ, Basinki DJ, et al. Normal polysomnographic values for children and adolescents. Am Rev Respir Dis. 1992;146(5 Pt 1):1235 –1239.
11. O’Brien LM, Mervis CB, Holbrook CR, et al. Neurobehavioral implications of habitual snoring in children. Pediatrics. 2004;114(1):44– 49.
12. Mitchell RB. Adenotonsillectomy for obstructive sleep apnea in children: outcome evaluated by pre-and postoperative polysomnography. Laryngoscope. 2007;117(10):1844–1854
13. Marcus CL. Childhood obstructive sleep apnea: to treat or not to treat, that is the question. Thorax. 2010;65(1):4–5
